Chapter 7: Immunology in Health and Medicine
Learning Objectives
By the end of this chapter you will be able to:
- Explain the deficiencies in immune function that can contribute to disease pathology.
- Classify hypersensitivities into four categories.
- Discuss testing, manifestations and treatments for hypersensitivity disease.
- Describe how components of the immune system are used in diagnostic techniques.
Case Study
Sarah, age 38, was diagnosed with rheumatoid arthritis (RA) at the age of 30. Rheumatoid arthritis involves the accumulation of antibodies within the joints as antibody-antigen complexes. Infiltration of immune cells and their interaction with immune complexes produces inflammation within the joint. Sarah initially presented with joint pain, stiffness, and swelling, predominantly in hands and wrists. Sarah underwent testing for rheumatoid factor, which is an antibody produced by some RA patients that binds IgG. This test involved observing agglutination of IgG-coated latex beads. An ELISA was performed to measure the amount of antibodies that bind Cyclic citrullinated peptide (anti-CCP). These antibodies may be produced because RA patients overproduce CCP within the joints. In addition to non-steroidal anti-inflammatory drugs (NSAIDs) and disease-modifying antirheumatic drugs (DMARDs) to reduce disease-associated inflammation, Sarah has received Adalimumab (Humira) therapy that involves infusion of a monoclonal antibody targeting tumor necrosis factor alpha (anti-TNF).
Sarah disease management is an ongoing process that involves periodic MRI scans to assess inflammation and tissue damage. However, with new advances in immunodiagnostics and immunotherapy, Sarah feels confident in being able to manage this complex immunological disorder.
- What type of hypersensitivity might rheumatoid arthritis be?
- What is the characteristic of immunoglobulins that causes IgG-conjugated latex beads to agglutinate in the presence of rheumatoid factor?
- What is the rationale for using monoclonal antibodies in immunotherapy for RA?
Answers to these questions are at the end of the chapter.
The immune system plays a critical role in preventing infection and repairing damaged tissues. However, the immune system is also a complex biological system that can adversely affect a person’s health when this system is perturbed. This chapter will discuss immune dysfunction and its effect on a person’s health as well as technologies that leverage the mechanisms of the immune system to diagnose and treat infection, cancer and immune disorders.
7.1 Immune Dysfunction
The immune system must maintain a balance between mounting an immune response to pathogens and immune tolerance to human cells and the microbiome. Immunopathology involves the study of disorders that emerge from disrupting this balance.
Immunopathologies fall into two categories:
Immunodeficiency occurs when the immune system fails to respond appropriately to pathogens or other threats. Deficiencies may emerge when the immune system is not completely developed or when it is suppressed or destroyed. For example, an individual may become immunodeficient as a consequence of cancer, since the immune response to cancer consumes resources that would be otherwise available to address infection.
Hypersensitivity occurs when the immune system responds too intensely or inappropriately to stimuli. Allergy involves an inappropriate immune response to environmental stimuli that do not usually pose risks to a person’s health. Autoimmune disease is an inappropriate immune response against a person’s own tissues. In the context of tissue graft and organ transplant, the immune response to the grafted tissue is considered to be a hypersensitivity as it is not a desirable outcome following a transplant.
Immunodeficiency
Immunodeficiencies are disorders associated with absent or functionally defective immune responses and may be either inherited before birth (“primary” or “congenital“) or acquired after birth (“secondary” or “acquired“).
Primary immunodeficiencies are typically inherited, however, the exact nature of the disorder is not always known.
Chronic granulomatous disease involves genetic defects that prevent phagocytes from producing antimicrobial superoxide. This disorder affects 1 in 200,000 people and is typically diagnosed in children (1-4 years old). These individuals are at higher risk for infection, particularly relating to catalase-positive bacteria (e.g. S. aureus, E. coli, Listeria) as well as Asprigillus and Candida fungus.
A person may produce low amounts of protective IgG antibody (hypogammaglobulinemia) or none at all (agammaglobulinemia). These individuals are at risk for frequent infection and are treated with immune serum globulin as well as continuous antibiotic therapy.
DiGeorge syndrome involves a defect in the development of the thymus, which results in a failure in T-cell development. The effect of this disorder is most apparent in the cell-mediated response because T-cells are involved as both inducers and effectors of this response. As a consequence, individuals with DiGeorge syndrome experience persistent fungal, protozoan and viral infections. In addition, since CD4 helper T-cells mature in the thymus and are necessary to activate B-cells, a person with DiGeorge syndrome may also lack antibodies. A thymus transplant can restore immune function for these individuals.
Severe combined immunodeficiency (SCID) describes the most severe form of immunodeficiency because affected individuals are unable to produce T-cells or B-cells. In one form of SCID known as adenosine deaminase (ADA) deficiency, developing lymphocytes lack adenosine deaminase, an enzyme needed to detoxify cells. X-SCID, where the affected gene is found on the X chromosome most frequently affects males. X-SCID involves a deficiency in interleukin receptors such that lymphocytes do not respond to the signals necessary to grow and become responsive. Since SCID places individuals at such high risk for recurrent infection patients will undergo a bone marrow transplant to replace their hematopoietic cells from a donor. While a bone marrow transplant has a success rate of 50% in curing SCID, there is a risk for graft-versus-host disease (GvHD) where T-cells within the bone marrow may induce an immune response against the new host. Donor bone marrow must be carefully processed to remove reactive T-cells prior to transplantation to reduce the risk of GvHD.
Secondary immunodeficiency typically arises as a consequence of infection (e.g. viral hepatitis or HIV infection), immunosuppressive therapy (e.g. cancer chemotherapy, radiation, graft rejection drugs) or prolonged disorders that impair normal body function (e.g. malnutrition, diabetes). Unlike primary immunodeficiencies that are typically a consequence of genetic defects, secondary immunodeficiency results from environmental and other exposures and may be reversible. However if untreated, individuals with secondary immunodeficiencies may have recurrent infections but also may develop rare cancers and opportunistic infections, which involves infection by microbes that are normally harmless (e.g. Candida yeast infection or Cryptosporidium diarrheal disease).
Acquired immunodeficiency syndrome (AIDS) is the best-known secondary immunodeficiency and is a consequence of infection by the human immunodeficiency virus (HIV). The HIV virus uses the CD4 protein as a viral receptor to attach to and enter helper T-cells. Infected T cells subsequently die of infection and through a cellular apoptosis response called pyroptosis. The profound decrease in CD4 T cells results in impairment of the adaptive immune response.
Hypersensitivity
Hypersensitivity involves an exaggerated or inappropriate immune response.
Hypersensitivities can be classified into four types:
Type I: Involve exposure to specific environmental antigens called allergens. The adaptive immune response to these allergens produces IgE antibodies as well as memory lymphocytes that perpetuate the disorder. IgE binds the surface of inflammatory cells, such as mast cells, which have internal granules containing histamine. Upon future exposure to the antigen, mast cells degranulate and the histamine is released to trigger inflammation.
Type II: Specific IgG and IgM antibodies are produced, which target cellular antigens. The target cells and tissues are damaged in the subsequent immune response, resulting in a loss of function for that particular tissue.
Type III: Antibodies and antigens agglutinate to form a web of immune complexes. These complexes leak into the bloodstream and deposit at various sites throughout the body. Where immune complexes accumulate, the local tissue becomes damaged and inflamed.
Type IV: T-cell–mediated reactions damage tissues through activation of macrophages and cytotoxic T cells. These reactions normally occur more than 12 hours after exposure to allergen, leading it to be called a delayed-type hypersensitivity.
Type I Hypersensitivity
Type I hypersensitivity has significant parallels to the standard adaptive immune response. The antigens that trigger type I hypersensitivity are called allergens and are typically harmless environmental substances, such as skin flakes (dander) from animals, pollen, molds or certain foods, such as peanut or shellfish.
Stage 1: Sensitization
As with the standard humoral immune response, allergen-specific Th2 cells activate B-cells that are also specific to the same allergen. Following clonal expansion, differentiation into plasma cells and IgM secretion, the B-cells undergo class switching. The divergence of an immune response and an allergy response arises because class-switching produces IgE-secreting B-cells. IgE is distributed in the body by the bloodstream and deposits on the surface of mast cells. This first exposure to allergen does not necessarily produce allergy symptoms but instead sensitizes a person to future potential allergy response.
Stage 2: Provocation
After IgE class switching and sensitization, exposure to allergen will cause the allergen to bind the IgE that have deposited on the mast cell surface. Granules inside the mast cell hold histamine and this histamine is released by a process called degranulation. Other factors like serotonin and bradykinin are also released by degranulation. Together, these inflammatory cytokines induce inflammation and allergy symptoms within 10-15 minutes of exposure. Activation of mast cells also induces metabolism of arachidonic acid, leading to the production of prostaglandins and leukotrienes. These cytokines can produce a more sustained allergy response.
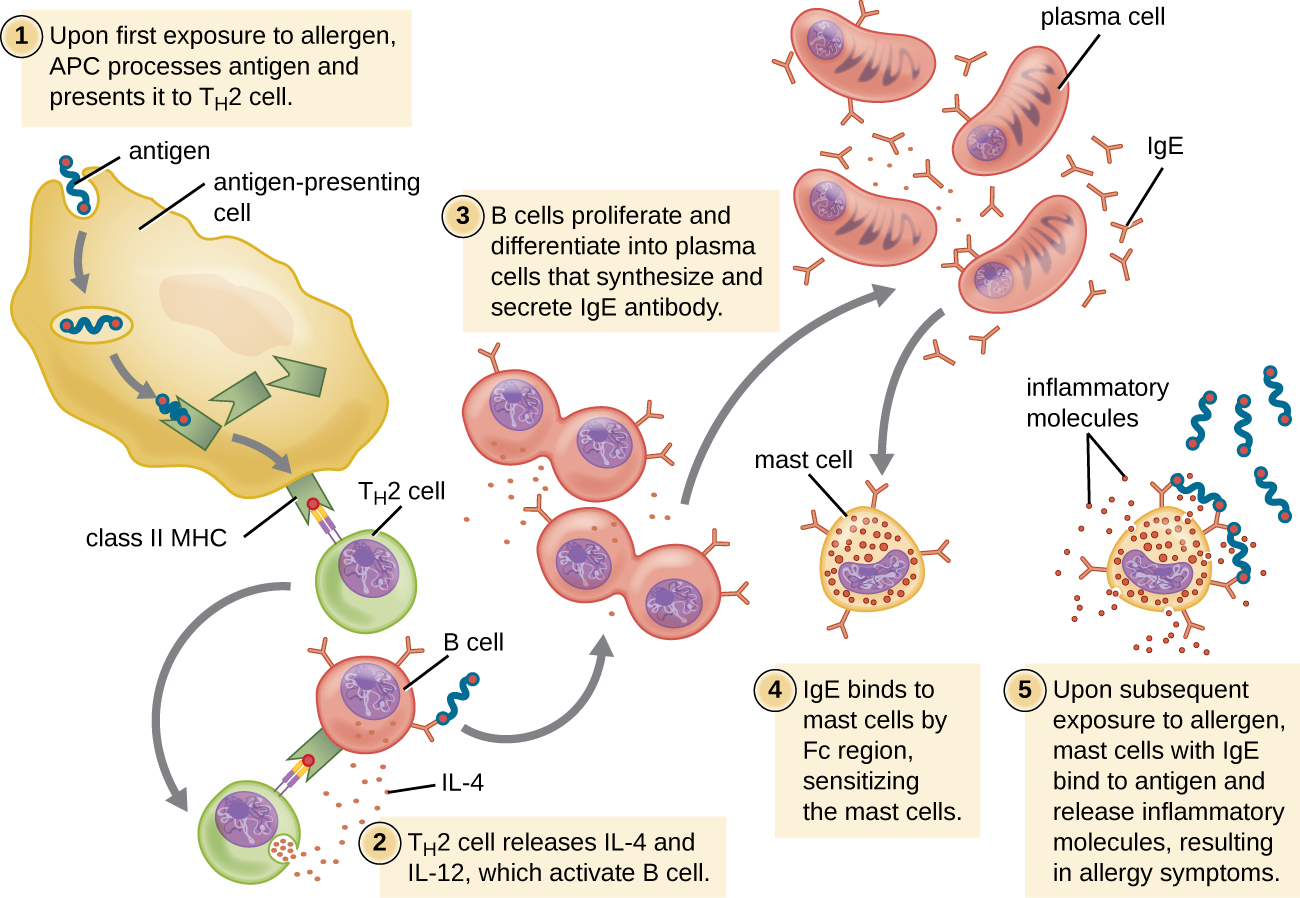
Figure 7-1 Allergy Sensitization and Provocation. The sensitization phase of allergy involves allergen detection by both Th2 and B-cells (1-2). The B-cells undergo class switching to secrete IgE and the IgE deposits on the surface of mast cells (3-4). The provocation phase of allergy occurs on subsequent exposure to allergen, where allergen binds to IgE on the mast cell surface and induces degranulation to release histamine and other inflammatory molecules (5). [Link to Image Description]
Image Source: By OpenStax CC BY 4.0, via Wikimedia Commons
Atopic Hypersensitivity Responses
Atopic diseases traditionally included asthma, eczema, and hay fever because they all run in families. However, the classification has since been expanded to describe the personal or familial tendency to produce IgE antibodies in response to allergens.
Atopic allergies may present as either local or systemic reactions. Local reactions include inflammation in a confined organ, such as airway inflammation of atopic asthma or skin irritation in allergic eczema (atopic dermatitis). A systemic response is called anaphylaxis and is characterized by inflammation in distinct organs and tissues throughout the body, resulting in swelling of the tongue and trachea, blockage of airways, and a dramatic drop in blood pressure leading to potentially fatal anaphylactic shock.
Allergy Therapy
Therapies for allergy responses are based on the mechanisms associated with this immunological process. Since allergies depend on plasma B-cell secretion of IgE, effective therapies can target the activity of the plasma cells (corticosteroids) or can reduce the systemic accumulation of IgE (anti-IgE antibodies). The IgE bind the surface of mast cells, priming the mast cell by acting as a de facto allergen-specific receptor. When primed mast cells interact with allergen, they degranulate to release histamine. Cromolyn acts to inhibit degranulation while anti-histamines block the histamine receptor. Non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen, can mitigate the inflammation that results from an allergic response.

Figure 7-2 Allergy Therapy. Allergens are environmental agents that induce plasma B-cells to secrete IgE (1). Corticosteroids and anti-IgE reduce the production and accumulation of IgE within the body (2). IgE binds to and primes mast cells, which are then sensitized to degranulate on exposure to allergen (3). Cromolyn inhibits mast cell degranulation while antihistamines block the action of histamine that is released through this process. NSAIDs also inhibit the inflammation that occurs during allergic response. [Link to Image Description]
Type II Hypersensitivity
Type II hypersensitivities involves IgM and IgG binding to human cells, followed by damage to those cells by lysis, phagocytosis and/or antibody-dependent cell-mediated cytotoxicity (ADCC). The surrounding tissue may become inflamed and type II hypersensitivities underlie most autoimmune diseases.
Blood Type Incompatibility
Blood type incompatibility may occur in response to blood transfusion or pregnancy and involves antibodies that eliminate or “reject” the non-self red blood cells. Blood types are determined by the presence or absence of specific antigens on the surface of red blood cells.
The two most widely known blood type systems are the ABO system and the Rh system.
ABO blood type is determine by the presence or absence of carbohydrates ‘A’ and ‘B’ on the red blood cell surface, where ‘O’ represents the absence of either carbohydrate. ABO blood type is inherited as a gene copy (allele) of the blood antigen from each parent, where genotype describes each gene copy. For example, AO indicates a person has one allele to produce surface carbohydrate A and an allele that does not produce carbohydrate antigen. Since, A-antigen is produced the red blood cell is A-type.
The specific genotypes and corresponding blood types are listed below:
- A-Type: AO, AA – red blood cells have only A carbohydrate on cell surface
- B-Type: BO, BB – red blood cells have only B carbohydrate on cell surface
- AB-Type: AB – red blood cells have both A and B carbohydrates on cell surface
- O-Type: OO – red blood cells have neither A nor B carbohydrates on cell surface
The immune system generates IgM antibodies, called isohemagglutinins, against red blood cells with blood group antigens not found on an individual’s own red blood cells. These antibodies are produced early in life and are maintained, such that red blood cell rejection could occur with every transfusion.
A person with A-type blood (AO or AA) would make antibodies against the foreign B-antigen (antibodies are called anti-B). Conversely, a person with AB-type blood would not make antibodies against either A-antigen or B-antigen. The AB-type individual is called the universal recipient because they can receive blood from any donor without rejection of blood on the basis of ABO blood group antigens. The O-type individual will reject RBCs from donors with every blood type except O-type. Importantly, individuals with O-type blood are regarded as universal donors because the absence of surface antigen allows the transfusion of their RBCs into persons of other ABO blood types, without rejection on the basis of these antigens.
ABO Blood Typing
See the Appendix A1-1 for more information on ABO Blood typing
Rhesus (Rh) factor blood type is described as the presence (Rh+) or absence (Rh-) of Rh factor (Rho/D antigen) on the surface of red blood cells. A person who is Rh+ can receive Rh- transfusion without consequence, because Rh- blood has no antigen.
A person who is Rh- and receives a transfusion with Rh+ blood will initiate a primary immune response. However, unlike the ABO blood group, anti-Rh IgMs do not pre-exist as such the rejection of transfusion is delayed by two weeks. Following the initial sensitizing event, subsequent transfusions will trigger a rapid and more potent secondary response involving IgG.
Rh-incompatibility must be considered during pregnancy if a Rh- mother is pregnant with a Rh+ fetus. During childbirth the mother’s immune system is likely to become sensitized toward the Rh antigen. In subsequent pregnancies, anti-Rh IgG produced by the mother and will cross the placenta resulting in red blood cell hemolysis in the fetus and the potentially life-threatening hemolytic disease of the newborn.
Through routine screening before and during pregnancy, affected mothers can be identified and treated with human Rho/D immune globulin (e.g., RhoGAM). RhoGAM is administered to the mother during the 28th week of their pregnancy and within 72 hours after delivery. These immunoglobulins function by binding and eliminating fetal Rh+ red blood cells before they come into contact with and sensitize the lymphocytes of the mother.
Drug-Induced Immune Hemolytic Anemia (DIIHA)
DIIHA is commonly observed when patients have been treated with penicillin and some cephalosporin class antibiotics. It is suspected that the antibiotic becomes attached to the surface of red blood cells. Antibodies (IgM or IgG) bind the antibiotics and mark the red blood cell for destruction by complement fixation and hemolysis. DIIHA depends on the presence of the drug and will disappear when the drug is discontinued.
Type II Hypersensitivity Autoimmune Disorders
Antibodies (IgM/IgG) may contribute to autoimmune disorders in multiple different ways. Antibodies may bind cell receptor proteins to turn on or off signals to the cell. For example, in Grave’s disease, autoantibodies bind and activate the receptors for thyroid stimulating hormone (TSH), which causes the thyroid to become hyper-activated and release excess thyroid hormones. Affected persons experience weight loss, rapid heartbeat, nervousness and related effects.
Alternatively, antibodies may bind human cells and cause damage to the tissues of the affected person. Hashimoto’s disease involves antibody-mediated damage to the thyroid that results in an underproduction of thyroid hormones leading to slowed heartbeat, fatigue, weight gain and other effects that contrast directly with Grave’s disease. Similar tissue dysfunction may occur from antibody-mediated damage to lungs and kidney basement membrane (Goodpasture’s syndrome), heart muscle (rheumatic fever), peripheral nerves (Guillain–Barré syndrome) as well as a range of other tissues.
Type III Hypersensitivity
Type III hypersensitivity results when antigen exists in a soluble form, not bound to the surface of a cell. This may occur as a consequence of some infections (e.g. post-streptococcal glomerulonephritis), reactions to serum or vaccine components, or diseases with genetic predisposition (systemic lupus erythematosus, rheumatoid arthritis).
Antibodies produced against these soluble antigens form antigen-antibody immune complexes that disseminate through the bloodstream and deposit throughout the body. Common sites of immune complex deposition include the glomerulus of the kidney, where blood is filtered, joints and in tissues with high oxygen demand and consequently develop networks of many small blood vessels (heart, lungs, brain, etc.). The affected tissues become inflamed and attract immune cells resulting in tissue destruction.
Type IV Hypersensitivity
Type IV hypersensitivities are regulated by T-cells, however, unlike the other hypersensitivity types, the effector cells are activated in an antibody-independent manner. Type IV hypersensitivities may be delayed-type hypersensitivities, where the immune response may occur up to 12 hours post-exposure to antigen. These immune hypersensitivities may occur when antigen is presented by antigen presenting cells (APCs) to induce a Th1-specific immune response. Subsequent stimulation of cytotoxic T-cells and monocytes/macrophages contribute to local inflammation and tissue damage.
- Contact dermatitis is an example where chemical agents on the skin bind to cells and proteins to produce a larger antigen (“hapten”) that sensitizes a person to that chemical. Upon future exposure, the chemical agent becomes the target of an Th1 immune response. Influx and stimulation of immune cells that secrete inflammatory cytokines induces swelling, itching and pain at the site of contact. Contact dermatitis resulting from contact with poison ivy is a specific example of this type of hypersensitivity.
- Tuberculin-type hypersensitivity is used as the basis of the tuberculosis skin test. Bacterial tuberculin protein is purified and administered by intradermal injection. Influx of inflammatory cells produces a local induration and swelling that is typically measured at 48-72 hours after the injection. The diameter of induration indicates the type four hypersensitivity that occurs if a person was previously exposed to Mycobacterium tuberculosis.
- Some organ transplant rejection is a consequence of type IV hypersensitivity. APCs present foreign antigen of the grafted tissue, resulting in a Th1 immune response. CD8 cytotoxic T-cells will be induced and will actively eliminate the transplanted tissue.
Autoimmunity and Autoimmune Disease
Autoimmunity is a complex and intriguing aspect of the immune system, involving the body’s defense mechanisms turning against its own tissues and cells. Low levels of autoimmunity is normally observed and may be involved in coordinating tissue development or elimination of old cells. However, if specific autoimmune responses become enhanced or dysregulated, a person may experience an autoimmune disease because of damage incurred on a specific tissue.
Autoimmune diseases are believed to be affected by a multitude of environmental, physiological and genetic factors as such many of the detailed mechanisms behind autoimmunity is still unknown. For example, autoimmune diseases are generally more frequently experienced by individuals of female biological sex. Environmental factors include infection and chemical exposure while major physiological drivers of autoimmunity include age, pregnancy and hormonal changes. Some autoimmune diseases are observed in individuals with a family history, suggesting a genetic component as well.
Normally, the immune system distinguishes between self and non-self, targeting foreign invaders while sparing the body’s own constituents. However, in autoimmune diseases, this self-recognition breaks down and immune cells mistakenly attack healthy tissues, which can result in chronic inflammation, tissue damage. There is a wide spectrum of autoimmune diseases, each characterized by specific targets. Conditions such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and multiple sclerosis exemplify the diverse array of autoimmune disorders, each with its unique clinical manifestations. Understanding autoimmunity and autoimmune diseases is crucial for developing therapies that modulate or suppress the aberrant immune responses and alleviate the suffering of affected individuals.
7.2 Immunodiagnostics and Immunotherapy
Antibodies as Tools
Antibodies play a critical role in the immune response, by marking pathogens and foreign agents for elimination from the body. A key characteristic of antibodies is their tremendous binding specificity, which emerges due to VDJ recombination. Their high specificity makes antibodies valuable tools for both detecting illnesses (immunodiagnostics) and treating inflammatory or infectious diseases (immunotherapy).
Antibody specificity is determined by the antigen binding site, which forms primarily from VDJ recombination. Each B-cell receptor destined to become an antibody has a unique amino acid conformation resulting in a three dimensional shape and chemical characteristics (non-covalent bonds) that allows them to interact specifically with complementary shapes and chemical characteristics on an epitope of the target antigen.
The strength of binding between an antibody binding site and the epitope of its target antigen is known as affinity. Affinity can be measured in a laboratory assay. However, in nature interactions between antibodies and antigens depend on more than just the antigen binding site and the epitope. In this case avidity, which accounts for the overall structural arrangement of the whole antibody and the antigen is a more relevant measure. Avidity takes into account the interactions between all antibody binding sites and multivalent antigens. The distinction between these terms is exemplified by IgG and IgM. The J-chain of IgM connects five immunoglobulin molecules together. Consequently, if IgG and IgM have the same affinity (binding of antigen binding site to epitope), the IgM will still exhibit higher avidity because the antibody has five-fold more antigen binding sites.
In some cases, two antigens may be structurally similar and antibodies that specifically target one antigen may inadvertently bind another antigen as well. This unintentional binding of an antigen is called cross-reactivity. One example of cross-reactivity is the herpes simplex virus 2 (HSV-2) IgM test for evidence of early infection by this sexually transmitted disease. A false positive detection of HSV-2 may occur if the person has been infected by HSV-1 (“cold sore” oral herpes), which easily transmitted without sexual contact. The reason that this test fails is that HSV-1 and HSV-2 viruses share structurally similar epitopes that would bind the antibodies.
Another example of cross-reactivity results from molecular-mimicry, which is a phenomenon where pathogens acquire epitopes that are structurally similar to those found in human tissues, either by chance or possible evolution to evade immune detection. For example, Streptococcus pyogenes M-protein has structural similarities to myosin protein of the human heart. Antibodies produced during S. pyogenes infection can produce an autoimmune response against human heart tissue, leading to development of rheumatic fever that persists long after the bacterial infection has been resolved.
Another characteristic of antibodies that is relevant to immunodiagnostics and immunotherapy relates to how the antibodies are obtained. The classical approach to produce antibody involves immunization of an animal, such as a rabbit or goat, with a specific antigen. The animal will produce antibodies against this foreign antigen. Serum is harvested from the animal via bleeding and contains the antigen-specific antibodies. In this context, the serum is called antiserum to reflect the antibodies contained within. The antiserum preparation may also be called a polyclonal antibody because the animal produced a mixture of antibodies against the variety of epitopes on the antigen surface.
Immunodiagnostics
The high specificity of antibodies makes them an excellent tool for detecting and quantifying a broad array of targets, from drugs to serum proteins to microorganisms. With in vitro assays, antibodies can be used to precipitate soluble antigens, agglutinate (clump) cells, opsonize and kill bacteria with the assistance of complement, and neutralize drugs, toxins, and viruses.
The functional utility of antibodies can be extended via conjugation. The chemical fusion of dyes, enzymes, toxins, etc. to an antibody produces a conjugate that has the antigen-specificity of an antibody but the acquired function of the attached molecule.
Immunodiagnostics can be employed in a range of applications:
Serotyping: Microbial species differ in their cell surface composition. Subtle variation in antigens can even occur in subpopulations of microbes in the same species, called serotypes. One example of a serotyping method uses bead-conjugated antibodies that will specifically bind to some microbes. Binding of the bead to the microbe also causes the beads themselves to clump together (agglutination).
Serological Testing: The frequently used “blood test” for infection is also known as a serological test. Like serotyping, these methods may use antibodies specific to pathogen in order to detect infection in the bloodstream. However, antibodies to identify human immune cells and cytokines can also play an important role in in determining the type as well as the stage of infection.
Serological testing can be used to test for a range of blood abnormalities:
Agglutination of red blood cells to monitor blood transfusion and infection
Hemagglutination assays take advantage of the agglutination (clumping) of red blood cells that is observed when they are bound by compatible antibodies. This agglutination can be used as a read-out for standard blood incompatibility testing (Appendix A1-1 and Appendix A1-2), testing for antibodies that emerge as a consequence of infection (Appendix A1-3) and determining the precise pathogen responsible for infection (Appendix A1-4).
Using red blood cell lysis to assess complement protein function
Since complement proteins are responsible for the lysis of red blood cells, this method can assess the function of classical complement pathway (Appendix A3-1) and alternative complement pathway (Appendix A3-2). Complement lysis can also be used to determine if a person has developed antibodies to a particular antigen (Appendix A3-3)
ELISA for quantification of pathogen or immune components
See the Appendix A5 for information on the ELISA methods to measure the amount of pathogen protein, antibodies or other molecules that may emerge during infection.
ELISPOT for quantification cytokine or antibody secretion
See the Appendix A6 for information on the ELISpot method that can test for a specific response from immune cells, such as the secretion of cytokines or antibodies in response to allergens, transplant tissues or other foreign materials. Immune cell secretions can confirm that these cells are responding to the foreign material and indicate the nature of that response.
Immunoblot/Western blot to capture protein size and identity.
See the Appendix A7 for information on Western blot method. This method is ideal when antibodies may cross-react with different proteins in the specimen. Confirming the size of the protein can ensure you are measuring the correct one.
Flow cytometry to count cells.
See the Appendix A8-1 for information on flow cytometry cell counting. Antibodies are used to fluorescence-label specific cells and then cytometry is used to count the number of cells that are labelled. This method is frequently used to assess the number of specific immune cells in blood in order to identify specific immune responses or possible immune deficiencies, as part of a complete blood cell count with differential (CBC-DIFF; Appendix A13-1).
Microscopy methods.
Antibodies may be used to visualize specific cells or cell structures by their conjugation with fluorescent dyes in immunofluorescence microscopy (Appendix A9) or to visualize cells with antibodies conjugated with enzymes that catalyze a localized colour change (Appendix A10).
Immunoprecipitation to visualize antigen.
Immunoprecipitation involves binding antigen and antibody molecules together into dense clumps that form a precipitate that is visible at the bottom of a tube or well (Appendix A11). This method can be modified to quantify antibodies or antigen in precipitin ring assays (Appendix A12-1) or immunodiffusion assays (Appendix A12-2). Immunoprecipitation may be observed as simply cloudiness or turbidity in a tube, as seen in the CRP assay (Appendix A13-2)
Immunotherapy
Antibodies produced in the laboratory can be used to harnesses the body’s immune system to combat diseases, including cancer and autoimmune disorders. Monoclonal antibody (mAb) therapies, like Rituximab, bind the surface of cancer cells and mark these cells for elimination by complement and phagocytes. Other mAb therapies, like Pembrolizumab, bind proteins on the surface of cells to modulate receptor function. In the context of Pembrolizumab, the PD-1 receptor on T-cells normally suppresses their function. Binding of this receptor by mAbs can preserve T-cell function. Moreover, antibodies are integral to the emerging field of theranostics, which combines therapy and diagnostics. In theranostics, antibodies can be radiolabelled for diagnostic monitoring of cancer, while conjugation of drug using a cleavable linker allows the drug to be simultaneously delivered to the target cell. For example, Brentuximab vedotin couples radiolabels or imaging agents with a drug payload that reduces the growth of lymphoma cancer cells. The versatility and specificity of antibodies make them potent tools in the development of novel immunotherapies and the advancement of precision medicine.
Summary
- Immunodeficiency may occur in two ways:
- Primary – defect in the development of immune cells or the production of immune components. Primary immunodeficiencies are inherited before birth.
- Secondary – defect in immune function due to the influence of environment, infection, certain medications, or other occurrences after birth.
- Hypersensitivities are excessive or inappropriate immune responses and are divided into four types:
- Type I – allergen-specific IgE-mediated response where mast cells or similar inflammatory cells degranulate to secrete histamine.
- Type II – IgM or IgG antibodies that target a person’s own tissues.
- Type III – IgG-antigen complexes that deposit within the body, leading to inflammation and tissue damage.
- Type IV – Damage to a person’s own tissues due to auto-reactive cytotoxic T-cells and dysregulation of macrophages.
- Autoimmunity is part of normal immune homeostasis, where immune cells identify a person’s own cells and eliminate ones that become old or non-functional. However, autoimmunity can be dysregulated to produce an autoimmune disease.
- Conjugation involves addition of dyes, enzyme or other functional components to antibodies to enable immunotherapy and immunodiagnostics.

