Chapter 11: Problems in the Development of Human Potential
DSM 5 – Neurodevelopmental and Schizophrenic Spectrum Disorders
The diagnosis of neurodevelopmental disorders is based on clinical and behavioral observations made during childhood and adolescence. These disorders are suspected to be the result of impairments in the brain or central nervous system resulting from heredity or problems occurring during fetal development. Debilitating neurodevelopmental disorders with known genetic causes are Down syndrome and fragile-X syndrome. Down syndrome (Figure 11.1) occurs when a child inherits a fragment or entire third copy of the 21st chromosome (Figure 11.2).
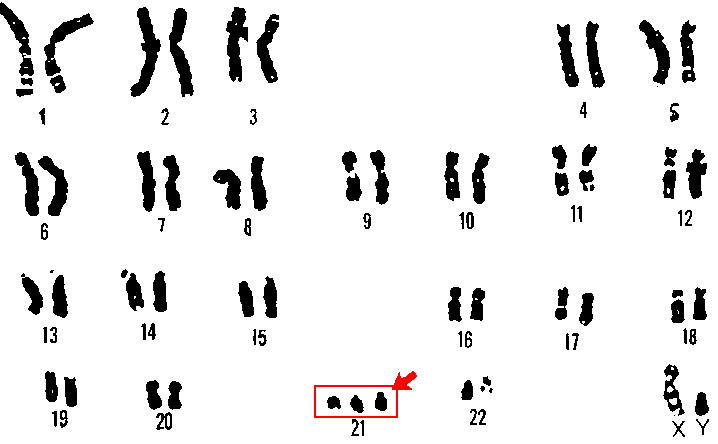
Figures 11.1 and 11.2 Chromosome 21 and Down’s syndrome.
Fragile-X syndrome results when there is a mutation of a known specific gene on the X chromosome (Santoro, Bray, & Warren, 2012). The following videos provide information regarding Fragile-X and autism spectrum disorders in young children.
Video
Watch the following video for information about Fragile X syndrome:
Video
Watch the following video of signs of autism:
The goal of psychiatry, to determine the biological mechanisms underlying DSM disorders, is gradually being realized. The initiatives in neuroscience described in Chapter 2, promise to speed up the acquisition of such knowledge. For example, it has recently been determined that autism results from an increase of patches of irregular cells in the frontal and temporal cortexes during fetal development (Stoner, Chow, & Boyle, et al., 2014). These are the parts of the brain involved in complex social relationships and language, both of which are problematic in those suffering from autism spectrum disorders. The parents of 11 autistic children who died donated their brain tissue for analysis. Recently developed imaging techniques detected irregular patches of cells in these areas in 10 of the 11 brains. In comparison, similar patches were observed in the brain tissue of these areas for only 1 of 11 children without autism. No such patches were discovered in the visual cortex for either sample. This is consistent with the fact that autistic individuals do not suffer from visual deficits (Stoner, Chow, & Boyle, et al., 2014). Such findings increase hope that advances in our understanding of the biological mechanisms underlying psychiatric disorders will result in more targeted and effective treatments in the future. At present, these disorders substantially impact a child’s potential intellectual, social, and vocational achievements.
DSM-5 incorporates several significant changes from previous editions. One important change was making the diagnosis of intellectual development disorder based on deficits in intellectual (e.g., language, reading, math), social (e.g., quality of friendships, interpersonal skills, empathy), and practical (e.g., personal grooming, time management, money management) functioning. In the past, scoring below 70 on an IQ-test was the exclusive criterion. Another significant change in DSM-5 is the collapsing of categories that had historically been sub-divided into types. For example, both autism and schizophrenia are now considered “spectrum” disorders requiring determination of severity rather than type. Figure 11.3 portrays the range of debilitation in autism spectrum disorders . Those diagnosed with Asperger’s syndrome or Pervasive Developmental Disorder in prior DSMs, are considered to be on the “mild” part of the spectrum. Those previously diagnosed as autistic are considered to be on the severe end of the spectrum, based on the nature and extent of behavioral symptomology and learning disability.

Figure 11.3 Autism spectrum disorders.
The previous categories of autism and schizophrenia spectrum disorders were collapsed because of the poor reliability of diagnoses for the sub-types of disorders. Reliability refers to the likelihood that two scorers arrive at the same diagnosis for an individual. For example, if two physicians took your temperature, they should both obtain the same reading. Otherwise, the thermometer would have no value. It has been demonstrated that psychiatrists are reliable in their diagnoses of the generic disorders (e.g., autism or schizophrenia) but not the different sub-types that had been listed in prior editions of the DSM (e.g., Asperger’s Syndrome, Pervasive Developmental Disorder, etc.).
Throughout this book we have seen the utility of the scientific method in establishing cause-effect relationships in psychology. We have come a long way in understanding how nature and nurture interact to influence feeling, thought, and behavior. Just as success in the basic sciences of physics and chemistry led to technologies enabling transformation of our environmental conditions, success in psychology has resulted in technologies of behavior change. For decades, practice in the helping professions, including psychology, was based on tradition, anecdotal evidence, and case studies. In the early 1990s, an approach to clinical practice based on application of the scientific method known as evidence-based practice emerged in medicine, psychology, education, nursing, and social work (Hjørland, 2011). The discipline of psychology only considers the results from experimentally controlled outcome studies including a plausible baseline control condition as credible evidence (Chambless & Hollon, 1998). The APA issued initial recommendations and later established a Task Force describing psychology’s commitment to evidence-based practice (American Psychological Association, 1995; APA Presidential Task Force on Evidence-Based Practice, 2006). The APA Division of Clinical Psychology maintains a website listing current evidence-based treatments for behavioral disorders (http://www.div12.org/PsychologicalTreatments/index.html). It is an excellent resource for determining the current state-of-the-art in clinical psychology.
Currently, there is no known effective medical treatment for autism spectrum disorders. It is hoped that progress in the neurosciences will produce effective interventions in the future. Until we are able to address the underlying biological mechanisms for the disorder(s), the best we can do is to try to address the behavioral symptoms. The learning-based treatment known as applied behavior analysis (ABA) has been successful in this regard. This approach will be described in depth in the following chapter. For now, it is important to note that even if a behavioral disorder stems from biological mechanisms, it can still be successfully treated with non-biological, learning-based procedures. The reverse may also be true. That is, in some instances it may be possible to address non-biological behavioral disorders medically, for example with drugs.
Video
Watch the following video for an introduction to applied behavior analysis (ABA):
The most commonly diagnosed DSM-5 neurodevelopmental disorder is attention deficit hyperactivity disorder (ADHD) , affecting approximately six percent of children all over the world (Wilcutt, 2012). ADHD is diagnosed when instances of attention-related problems (e.g., distractibility, daydreaming, etc.) occur in multiple settings. Inattentive children tend to have more difficulty in school than at home or with friends whereas the reverse is true for impulsive children who benefit from structure (Biederman, 1998). ADHD is diagnosed three times as often in boys than girls, resulting in controversy (Sciutto, Nolfi, & Bluhm, 2004). Adolescents and adults frequently learn to cope on their own (Gentile, Atiq, & Gillig, 2004).
ADHD is our first example of the concern expressed by Szasz regarding the appropriateness of applying the medical model to behaviorally-defined problems. Attentional problems are inferred from distractibility, inability to maintain focus on a single task, becoming bored with non-pleasurable activities, daydreaming, or not paying attention to instructions. Hyperactivity can be inferred from fidgeting in one’s seat, non-stop talking, blurting things out, jumping up and down, or impatience. All of these examples of attentional and hyperactivity problems are characteristic of practically all children. There is a saying that “if the only tool you have is a hammer, every problem that comes along looks like a nail.” Psychiatrists are trained as physicians to diagnose and treat illnesses. Treatment usually consists of prescribing medication. Many question the validity of considering ADHD a psychiatric disorder and the ethics of prescribing medications for so many children (Mayes, Bagwell, & Erkulwater, 2008; Schonwald & Lechner, 2006; Singh, 2008). Szasz (2001, p. 212) concluded that ADHD “was invented and not discovered.”
Two comprehensive literature reviews of experimental studies found learning-based treatment effective with children diagnosed as ADHD (Fabiano, Pelham, Coles, Gnagy, Chronis-Tuscano, & O’Connor, 2009; Pelham & Fabiano, 2008). A multi-faceted approach including parent training, teacher-parent classroom intervention, and an individualized program addressing independent work habits and social skills, has demonstrated significant improvements in ADHD second- through fifth-graders (Pfiffner, Villodas, Kaiser, Rooney, & McBurnett, 2013). Learning-based approaches to improving school performance will be described in more detail in the next chapter as we consider the role of professional psychologists in enabling individuals to achieve their potential in different environments.
Schizophrenia Spectrum Disorders
Schizophrenia is probably the DSM diagnosis most resembling the stereotype of “mental illness.” It is a disabling disorder characterized by severe cognitive and emotional disturbances. Schizophrenia is most likely to first appear late in adolescence or in early adulthood (van Os & Kapur, 2009). The symptoms are unusual and often bizarre. They may include delusions, hallucinations, disorganized speech, catatonic behavior, or flat affect (American Psychiatric Association, 2013). Delusions are strongly held beliefs having no basis in fact. One common delusion is that one’s behavior is being controlled by external forces (e.g., electric wires or “aliens”). Another is the belief that one has exceptional qualities or talents (i.e., delusions of grandeur). Hallucinations are inferred when an individual behaves as though a non-apparent event is occurring; for example, speaking to someone who is not present. “Word salad”, in which words are spoken in a meaningless fashion, is a common form of disorganized speech. Catatonia is a state of immobilization which can occur for a variety of reasons, including stroke, infection, or withdrawal from addictive substances. Sometimes an individual diagnosed with schizophrenia assumes the posture of a “waxy figure”, remaining still unless manipulated by another person. Flat affect refers to the lacking of emotional expression; the individual does not appear to experience emotions appropriate to the situation. Schizophrenia is commonly misunderstood as referring to a “split personality.” What had been diagnosed as Multiple Personality Disorder in previous editions of the DSM is now considered Dissociative Personality Disorder, and will be discussed below.
Schizophrenia is a chronic disorder with between 80 and 90 percent of the patients retaining the diagnosis over a ten-year period (Haahr, Friis, Larsen, Melle., Johannessen, Opjordsmoen, Simonsen, Rund, Vaglum, & McGlashan, 2008). In extreme forms, schizophrenia can be debilitating. The differences appear to reflect influences by both nature and nurture. The risk of developing schizophrenia increases as a function of the percentage of genes shared (nature) as well as similarity of environment (nurture). Identical twins are almost three times as likely to develop schizophrenia as fraternal twins. Fraternal twins as well as ordinary siblings share half their genes. Fraternal twins are likely to have more similar environments than ordinary siblings and are twice as likely to develop schizophrenia (Gottesman, 1991). Unlike Down and Fragile X syndromes, several genes are thought to be involved in schizophrenia (Picchioni & Murray, 2007).
In 1955, approximately 550 thousand Americans were housed in public psychiatric institutions. Development of anti-psychotic medications and implementation of federally funded treatment programs resulted in a dramatic reduction in this population to 100,00 by 1985 (Torrey, 1991). An unfortunate byproduct of this deinstitutionalization was that many patients diagnosed as schizophrenic were imprisoned or left homeless, without treatment (Eisenberg & Guttmacher, 2010).
The psychological model of maladaptive behavior, described later, distinguishes between behavioral excesses and behavioral deficits . A similar distinction is often made by psychiatrists between positive (i.e., excesses) and negative (i.e. deficits) symptoms of schizophrenia. Reports of delusions, hallucinations, or disordered speech are examples of schizophrenic behavioral excesses (positive symptoms). Behavioral deficits can include flat affect (i.e., little emotionality), poor interpersonal skills, and lack of motivation to succeed. Although behavioral deficits may be less disturbing than behavioral excesses, they actually interfere to a greater extent with daily functioning and are less responsive to medication (Smith, Weston, & Lieberman, 2010; Velligan, Mahurin, Diamond, et al. (1997). Medication suppresses delusions and hallucinations but cannot teach interpersonal skills or motivate an individual to achieve their potential. Although they are limited to positive symptoms, drugs still remain an effective approach to treating those diagnosed as schizophrenic (National Collaborating Centre for Mental Health, 2009).
Prior to deinstitutionalization, token economy procedures based on direct and indirect learning principles were successfully applied to schizophrenic populations within large psychiatric facilities (Ayllon & Azrin, 1968; Kazdin, 1977; Paul & Lentz, 1978). Token economies establish contingencies between a tangible generalized reinforcer (i.e. token) and desirable behaviors. Usually, a type of “store” is established, permitting the exchange of tokens for desirable items or opportunities to engage in pleasurable activities (Martin & Pear, 2011, pp. 305-319). After the drastic decline in inpatients resulting from use of anti-psychotic medications, there was a corresponding decline in the need for token economies in institutional settings. Still, additional treatment was necessary to address the behavioral and motivational deficits typically remaining after schizophrenics were released.
In a seminal study, therapy in which families were taught to manage the symptoms of schizophrenia (e.g., by monitoring compliance with taking medications, reducing stress, providing support) combined with medication, was shown to reduce relapse rates beyond that attained with medication alone (Goldstein, Rodnick, Evans, May, & Steinberg, 1978). Medication alone resulted in a 25% reduction in relapse in comparison to the placebo control and the addition of family therapy reduced relapse by an additional 25% (Dixon, Adams, & Lucksted, 2000; Dixon & Lehman, 1995).
Comprehensive reviews of controlled outcome studies evaluating cognitive-behavioral and family intervention treatments in which schizophrenics were taught to re-evaluate their symptoms, develop coping strategies, and engage in reality testing exercises, concluded these approaches were effective for treating negative as well as positive symptoms of schizophrenia (Jauhar, McKenna, Radua, Fung, Salvador, & Laws, 2014; Pilling, Bebbington, Kuipers, Garety, Geddes, Orbach, & Morgan, 2002; Rector & Beck, 2001; Turkington, Dudley, Warman, & Beck, 2004; Wykes, Steel, Everitt, & Tarrier, 2008). In addition, it has been found that fewer drop out of treatment, or relapse afterward, with the learning-based treatment approaches in comparison to when treated exclusively with anti-psychotic medications (Gould, Mueser, Bolton, et al., 2001; Rathod & Kingdon, 2010).
An example of the synergy between psychology and psychiatry is the relationship between basic research in cognition (see Chapter 7) and our current understanding of the nature of the intellectual deficits characterizing different DSM disorders. For example, the percentage of normal functioning for verbal memory, short-term (working) memory, psychomotor speed and coordination, processing speed, verbal fluency, and executive functioning were compared for low- and high-performing schizophrenics (Bechi, Spangaro, Agostoni, Bosinelli, Buonocore, Bianchi, Cocchi, Guglielmino, et. al, 2019).
Attributions
Figure 11.1 “Down’s syndrome” by Vanellus Foto is licensed under CC BY-SA 3.0
Figure 11.2 “Down’s syndrome and chromosome 21”, National Human Genome Research Institute is in the Public Domain
Figure 11.3 “Autism spectrum disorders” by Anwer2007 is licensed under CC BY-SA 4.0
based on clinical and behavioral observations made during childhood and adolescence; suspected to be the result of impairments in the brain or central nervous system resulting from heredity or problems occurring during fetal development
neurodevelopmental disorder that occurs when a child inherits a fragment or entire third copy of the 21st chromosome
neurodevelopmental disorder that results when there is a mutation of a known specific gene on the X chromosome
based on the nature and extent of behavioral symptomology and learning disability; Asperger’s syndrome is on the “mild” part of the spectrum and those diagnosed as autistic are considered to be on the severe end of the spectrum
the likelihood that two scorers arrive at the same diagnosis for an individual
learning-based approach to assessing and treating behavioral problems
diagnosed when instances of attention-related problems (e.g., distractibility, daydreaming, etc.) occur in multiple settings
disabling disorder characterized by severe cognitive and emotional disturbances
behaviors that occur more or less frequently than desired
establishes contingencies between a tangible generalized reinforcer (token) and desirable behaviors; tokens can be exchangeed for desirable items or opportunities to engage in pleasurable activities

