Chapter 11: Problems in the Development of Human Potential
DSM 5 – Bipolar, Depressive and Anxiety Disorders
Bipolar and Related Disorders
The importance of nature (heredity and biology) in neurodevelopmental and schizophrenia spectrum disorders is readily apparent. Neurodevelopmental disorders appear too early in life for nurture to have a major influence and the symptoms can be physical as well as behavioral. For example, Down syndrome children have distinct anatomical features making them easy to identify. Autistic (including many fragile X) children and schizophrenic adults are usually physically indistinguishable from their peers; however their defining symptoms are extreme and easily identifiable. Individuals with these diagnoses appear to differ from “normal” individuals qualitatively rather than quantitatively. Although it has been proposed in the past (c.f., Kanner, 1943), there is no evidence to suggest that faulty parenting is the cause of autism or schizophrenia. Rather, the evidence supports attributing these severe disorders to an underlying biological problem (Centers for Disease Control, 2011, p. 7).
Bipolar disorders are not as obviously influenced by hereditary and biological factors as neurodevelopmental and schizophrenia spectrum disorders. Those diagnosed with bipolar disorders may appear to differ from others in the extremity, rather than in the type of behavior. The defining characteristic of bipolar disorder is extreme excitability and irritability, referred to as mania. Extreme mania can result in risky life decisions and sleep disorders (Beentjes, Goossens, & Poslawsky, 2012). Figure 11.4 includes sketches of mood changes over a two-month period for individuals displaying the normal pattern as well as those of unipolar depression, bipolar types 1 and 2 as well as cyclothymia. The average person demonstrates relatively mild highs and lows. Unipolar depression is characterized by extreme lows. Bipolar 1 includes extended periods of extreme highs and lows whereas the high is not as extreme in bipolar 2. Cyclothymia is characterized by less severe and more frequent mood swings.
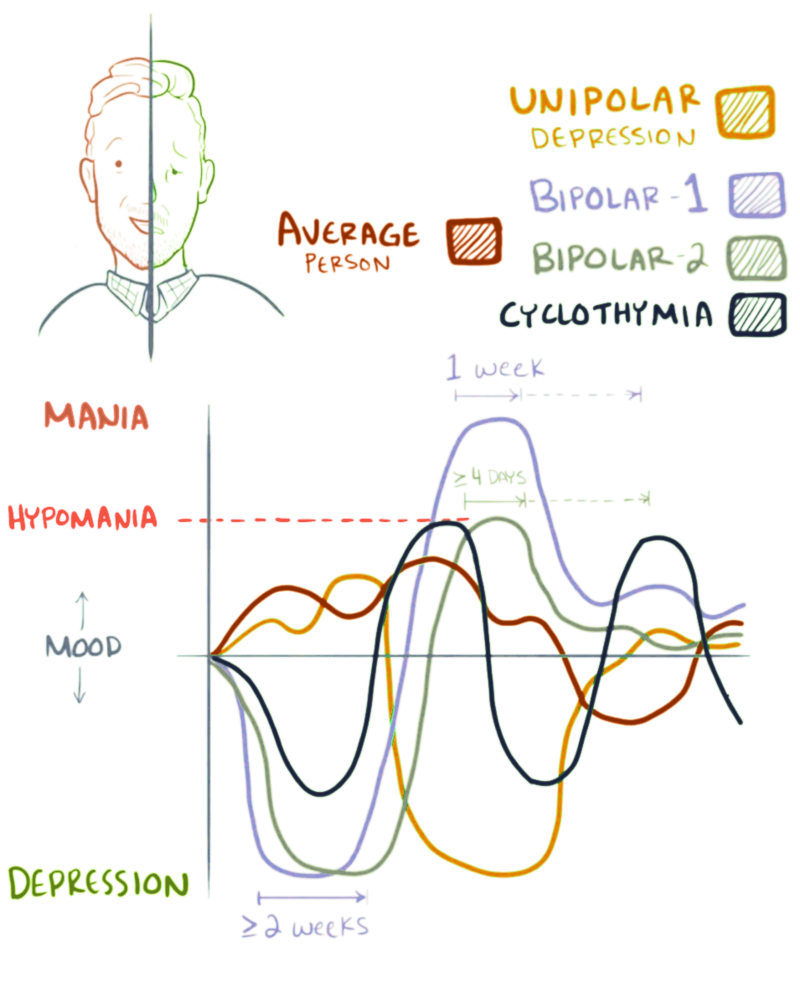
Figure 11.4 Bipolar disorder
Every one experiences “ups” and “downs” in life. Bipolar disorders involve more extreme moods and more frequent mood swings. One’s emotions usually reflect ongoing events in everyday life. The ups and downs of individuals diagnosed as bipolar may be episodic and not dependent upon environmental events. The episodes can be extreme and last as long as six months (Titmarsh, 2013). Evidence suggests there is a genetic component to bipolar disorder. First degree relatives (i.e. parents, offspring, and siblings) are ten times as likely to develop the disorder as the general population (Barnett & Smoller, 2009). Several genes appear mildly to moderately involved (Kerner, 2014). Pharmacologic treatment is often prescribed. Lithium thus far appears to be the most effective drug, particularly for reducing the frequency and intensity of manic episodes (Poolsup, Li Wan Po, & de Oliveira, 2000).
Depressive Disorders
Into every life a little rain must fall.
It is normal to experience sadness and different degrees of depression. Just as manic episodes can be extreme, the same is true for depressive episodes. Depression can be long-lasting and severe in its impact upon everyday functioning. The following are the DSM-5 diagnostic criteria for major depressive disorder :
At least five of the following symptoms have been present during the same 2-week period and represent a change from previous functioning: at least one of the symptoms is either 1) depressed mood or 2) loss of interest or pleasure.
- Depressed mood most of the day, nearly every day, as indicated either by subjective report (e.g., feels sad or empty) or observation made by others (e.g., appears tearful)
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated either by subjective account or observation made by others)
- Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day
- Insomnia or hypersomnia nearly every day
- Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down)
- Fatigue or loss of energy nearly every day
- Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick)
- Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others)
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or specific plan for committing suicide (American Psychiatric Association, 2013).
Due to its high rate of occurrence, major depressive disorder is often referred to as “the common cold of mental illness” (Seligman, 1975). A two-to-one female/male ratio of the incidence of depression has been found across nationality, culture, and ethnicity (Nolen-Hoeskema, 1990). In a review of research addressing these gender differences, Nolen-Hoeskema (2001) cited the higher incidence of the following factors for women; sexual assault during childhood, poverty, and greater responsibilities for child and parental care. She also describes differences in the characteristic ways males and females respond to stressful or disappointing situations. Women are more likely to maintain conscious focus on upsetting events (i.e., ruminate) whereas men are more likely to distract themselves or take action to address the situation (Nolen-Hoeskema, 2001). In the next chapter, we will describe the thinking patterns that are characteristic of those diagnosed with major depressive disorder and the cognitive-behavioral psychological treatments designed to modify these self-defeating patterns. Cognitive-behavioral treatments have been found to be as effective as pharmacological treatments for the short-term treatment of depression and to be more effective in maintaining treatment effects once drugs are withdrawn (Dobson, 1989). Anti-depressive medications may be prescribed for long-lasting episodes or when there are signs of suicidal thinking.
There is consensus among psychologists and psychiatrists that a nature/nurture model is necessary for understanding depression. The popular diathesis-stress model proposes that individuals vary in their susceptibility to depression based on interactions between their genetics and experiences, particularly during childhood (National Institute of Mental Health, 1999). In support of this model, it has been found that variation in the 5-HTT gene influencing the neurotransmitter serotonin increases the likelihood of becoming depressed after experiencing stressful life events (Caspi, Sugden, & Moffitt, 2003). The most popular anti-depressant medications are serum serotonin reuptake inhibitors (SSRIs) that affect the balance of the neurotransmitters serotonin, dopamine, and norepinephrine (Nutt, 2008). By inhibiting the reuptake of serotonin, its level is increased in the synaptic cleft enabling it to bind with other neurotransmitter receptor cells (see Figure 11.5).

Figure 11.5 How SSRIs work.
Anxiety Disorders
The transition from high school to college can be very stressful. It requires adapting to a different environment with a host of new responsibilities. If you are not commuting from home, it may be the first time in your life you are living on your own. Your parents are not waking you up in the morning and making sure you are on time for all your scheduled activities. They are not preparing your meals or checking to make sure you did your homework. You probably are experiencing more autonomy and perhaps more problems to solve on your own than ever before.
As we saw in Chapter 5, adaptive learning involves acquiring the ability to predict and where possible, control environmental events. After one is able to predict events, they no longer are surprised or anxious. Anxiety is the name for the feeling that one experiences in anticipation of a possible aversive event. When extreme, anxiety can be accompanied by activation of the autonomic fight-or-flight response including increases in one’s heart rate and rapid breathing. Once one becomes confident they can control events they no longer feel anxious and these physical responses subside. Do you remember your first days on campus when everything was new? How about your first exams? Did it matter what courses your exams were in or did you feel the same about all of them? How did you feel about approaching and speaking to your professors? Do you still feel the same way? I hope you have successfully adjusted to the rhythms and responsibilities of college life. If so, you probably feel a lot less anxious than you did those first days on campus.
The major anxiety disorders listed in DSM-5 include the following:
- Generalized Anxiety Disorder
- Specific Phobia
- Social Anxiety Disorder (Social Phobia)
- Panic Disorder
Just as we all experience ups and downs, we all experience anxiety and fear. Once again, only when it reaches the point where it interferes with our daily functioning and ability to enjoy life on an ongoing basis, does extreme anxiety or fear become diagnosed as a psychiatric condition. Generalized anxiety disorder occurs across many situations and is chronic. Anxiety and fear are modulated by the primitive part of the brain called the limbic system that was described in chapter 2. General anxiety disorder is thought to be the result of faulty processing of fear between the amygdala and the hypothalamus, brain stem, and cerebellum (Etkin, Prater, Schatzberg, Menon, & Greicius, 2009). These areas are involved in determining the threat level of a stimulus and relaying the information to the cortex for higher-level processing and formulation of a response. Functional MRI imaging was conducted on normal subjects and those suffering from general anxiety disorder. The connections between the amygdala and other brain areas were significantly less distinct in those suffering from the disorder whereas there was increased cortical connectivity. The authors concluded that these results supported a model of general anxiety disorder in which those affected with malfunctioning amygdala were forced to compensate at higher levels of the cortex (Etkin, Prater, Schatzberg, Menon, & Greicius, 2009). Consistent with this cognitive interpretation of general anxiety disorder, as with depression, an extensive review of experimental research evaluating cognitive-behavioral and pharmacologic treatment approaches found them comparable in their short-term effects. Cognitive-behavioral procedures, however, once again demonstrated long-lasting effects whereas pharmacologic improvements disappeared once medication was terminated (Gould, Otto, Pollack, & Yap, 1997).
Unlike general anxiety disorder, which occurs in many situations, the diagnosis of a specific phobia pplies to an extreme and irrational fear occurring in a specific situation. Common examples of easily acquired fears related to our evolutionary history include spiders, snakes, height, open spaces, confined spaces, strangers, and dead things (Seligman, 1971). Social anxiety disorder (social phobia) refers to extreme and irrational anxiety related to real or imagined situations involving other people. It often involves circumstances in which one is being assessed or judged (e.g., in school, at a party, during interviews, etc.). As described in Chapter 5, desensitization and reality therapy procedures are very effective in treating anxiety and fear disorders. Self-help techniques based on cognitive behavioral strategies have been found effective for some individuals (Lewis, Pearce, & Bisson, 2012).
Panic attacks are unpredictable and can be debilitating. Physical symptoms may include a rapid pulse, shortness of breath, perspiration, and trembling. Symptoms can be so severe as to be interpreted as a heart attack. The person can feel as though they are losing control, going crazy, or dying. Pharmacologic treatment and cognitive behavioral techniques have both been found to be more effective than placebos for the treatment of panic disorders, with the combination producing the best results (van Apeldoorn, van Hout, Mersch, Huisman, Slaap, Hale, & den Boer, 2008).
Obsessive-Compulsive and Related Disorders
Obsessions are thoughts that repeatedly intrude upon one’s conscious experience. Compulsions are behaviors one feels the need to repeat despite their interfering with achievement of other tasks. Historically, there has been confusion regarding the different ways in which these terms are used in DSM diagnoses. The distinction is still made in DSM-5 between obsessive-compulsive disorder (OCD) and obsessive-compulsive personality disorder (OCPD); the latter will be treated separately under personality disorders. OCD and OCPD can include repetitious behaviors such as hoarding or placing things in neat piles. The OCD individual recognizes these behaviors as problematic whereas the OCPD individual sees them as being appropriate and desirable. OCD is sometimes considered an anxiety disorder with the ritualistic behaviors maintained by stress-reduction (i.e., negative reinforcement). Similar to depression and other anxiety-related disorders, OCD has been successfully treated with SSRIs. The cognitive behavioral technique, exposure and response prevention has been found highly effective in the treatment of OCD (Huppert & Roth, 2003). For example, if a person constantly checks to see if a door is locked, they are permitted to check only once (i.e., they are exposed to the lock and prevented from making the response a second time). A major research study found that exposure and response prevention was as effective alone as when it was combined with medication for OCD (Foa, Liebowitz, Kozak, Davies, Campeas, Franklin, Huppert, Kjernisted, et al., 2005).
Trauma- and Stressor-Related Disorders
Posttraumatic stress disorder (PTSD) may be acquired through a direct or indirect learning experience. One can experience a traumatic event such as sexual assault, severe injury, or threat of death; or one can observe any of these events occur to someone else, particularly a close friend or relative. Diagnosis of PTSD is usually made when a person reports experiencing recurrent flashbacks of a traumatic event more than a month after it happened. The person may avoid talking about or approaching any reminder of the event (American Psychiatric Association, 2013).
Similar to major depressive disorder, a diathesis-stress model appears to apply, there being evidence for individual differences in susceptibility to PTSD. In this instance, genes effecting the neurotransmitter GABA were found to be related to the likelihood that individuals experiencing severe trauma as children were diagnosed with PTSD as adults (Skelton, Ressler, Norrholm, Jovanovic, & Bradley-Davino, 2012). Similar findings were obtained with adults who were abused as children. Those having a particular gene were more likely to later develop PTSD (Binder, Bradley, & Liu, 2008). Cognitive-behavior therapy is considered the treatment of choice for PTSD by the United States Departments of Defense (Hassija & Gray, 2007) and Veteran Affairs (Karlin, Ruzek, Chard, Eftekhari, Monson, Hembree, Resick, Foa, & Patricia, 2010).
Attributions
Figure 11.4 “Bipolar disorder” is licensed under CC BY-SA 4.0
Figure 11.5 “SSRI mechanisms” by Sabar is in the Public Domain, CC0
characterized by extreme excitability and irritability (mania); bipolar 1 includes extended periods of extreme highs and lows whereas the high is not as extreme in bipolar 2; cyclothymia is characterized by less severe and more frequent mood swings.
sadness or emptiness most of the day and/or markedly diminished interest or pleasure in activities
empirically validated talking therapy procedures based on psychological principles
assumes that individuals vary in their susceptibility to the effects of stress
popular anti-depressant medications that affect the balance of the neurotransmitters serotonin, dopamine, and norepinephrine; by inhibiting the reuptake of serotonin, its level is increased in the synaptic cleft enabling it to bind with other neurotransmitter receptor cells
the feeling that one experiences in anticipation of a possible aversive event
chronic anxiety occurring across many situations
an extreme and irrational fear occurring in a specific situation
extreme and irrational anxiety related to real or imagined situations involving other people
unpredictable, debilitating anxiety; physical symptoms may include a rapid pulse, shortness of breath, perspiration, and trembling
thoughts that repeatedly intrude upon one’s conscious experience
behaviors one feels the need to repeat despite their interfering with achievement of other tasks
disorder characterized by repetitious behaviors such as hoarding or placing things in neat piles
person reports experiencing recurrent flashbacks of a traumatic event more than a month after it happened; person avoids talking about or approaching any reminder of the event

