Chapter 10. Tubes and Devices
10.5 Tracheostomies
Tracheostomy Tubes
Tracheostomy tubes (TTs) are artificial airways that can be permanent or temporary depending on the patient’s condition. They are placed through a hole in the neck and into the trachea to overcome tracheal obstruction caused by head and neck trauma including surgery or tumour. Other reasons for tracheostomy tubes include the need for prolonged mechanical ventilation and/or when the client is unable to maintain a patent airway because of conditions like neuromuscular disease or spinal cord injury (BTS, 2014; Perry et al., 2018; RCH, n.d.).
Nursing care of clients with tracheostomy tubes varies depending on how well established the tracheotomy is. The British Thoracic Society prioritizes humidification, ensuring the cleanliness and patency of the inner tube, secure fixation of the tube, and attention to cuff pressure as necessary for preventing TT related complications (BTS, 2014).
If the trach is temporary, decannulation (or removal) should be done as soon as possible to reduce the risk of complications. Decannulation should only be done by competent persons and is only done following thorough assessment of the upper airway.
 |
 |
Tracheostomy tubes can be soft plastic, hard plastic, or, at times, metal. All tracheostomy devices are made up of a number of pieces. Understanding the structure and function is key to providing safe trach care. (See Figure 10.2 and Table 10.2.) TTs come in different sizes and may have a cuff and may be fenestrated. A cuffed tracheostomy produces a tight seal between the tube and the trachea. This seal prevents aspiration of oropharyngeal secretions and air leakages between the tube and the trachea. Tracheostomies are firmly tied and secured around the patient’s neck. The ties prevent accidental decannulation of the trachea (in other words, accidental trach removal). New tracheostomies require attention to principles of asepsis for stoma (wound) care. Tracheostomies that are well established require clean technique for stoma care.

Table 10.2 Parts of a Tracheostomy Tube |
|
| Outer cannula | Sits in the trachea |
| Inner cannula | Fits inside the outer cannula. It is a safety feature and can be removed and replaced if obstructed. Whenever possible, TT that include an inner cannula should be used. |
| Flange / face plate | Rests against the patient’s neck. Prevents the TT from migrating into the trachea. |
| Obturator | Sits inside the TT and is used when the TT is situated. It is replaced with an inner cannula. |
| Cuff | When inflated, provides protection from aspiration. Prevents the escape of air between the tube and tracheal wall. Cuff pressures that are too high can damage the tracheal mucosa. Follow your agency guidelines for monitoring cuff pressure. A note about uncuffed TTs: they allow patients some control with clearing their own airway, but they present increased risk of aspiration. Uncuffed TTs allow some patients to speak when the tube is in place. |
| Pilot balloon / cuff inflation line | Controls the inflation, deflation of the cuff. |
| Data source: BTS, 2014 | |
Figure 10.3 shows a cuffed TT in situ (in place). Note the flow of air only occurs in and out of the TT. People with these kinds of TTs cannot talk because no air is allowed to pass the larynx. Figure 10.4 shows an uncuffed TT in situ. The flow of air occurs in and out of the TT and through the natural airway. People with these kinds of TTs can talk by covering the trach tube opening to force all expired air through the larynx.
 |
 |
Fenestrated TTs have a number of holes in the outer cannula to allow air to flow from the lungs over the vocal cords. They can be used in conjunction with an uncuffed TT often when weaning the patient from the TT. They are only to be used with patients who can swallow without risk of aspiration (St. George’s University Hospital, n.d.).

Other considerations for persons with TTs:
- Patients often need to lie at a 30-degree, or greater, angle to facilitate breathing and lung expansion.
- All persons with a tracheostomy must have suction equipment and emergency supplies at the bedside. Emergency equipment is usually in a clear bag on an IV pole attached to the patient’s bed.
- People with tracheostomies cannot eat or drink (and often have difficulty swallowing) when the cuff is inflated. These people are NPO because of risk of aspiration.
- People with cuffed tracheostomies cannot talk because air cannot bypasses the larynx. As such, finding alternative forms of communication is paramount. For some, a permanent tracheostomy has led them to acquire a speaking valve (BTS, 2014). Others may use fenestrated TTs to help them communicate through speech (The Ohio State University Wexner Medical Center, 2012). (See Figure 10.5.)
- People with a tracheostomy must always have the tracheostomy tied securely around the neck using ties, according to agency policy. This prevents the tube from accidentally falling out.
- Patients with a tracheostomy produce more secretions than usual and may not be able to clear secretions from the tracheostomy with coughing. If secretions in the tracheostomy impair air entry and cause respiratory distress, the patient should be suctioned immediately.
- Persons who breathe through a tracheostomy bypass the upper airway where moisture is added to the breath. As such, dry air can dry out airways and cause possible tube blockage from tenacious sputum. Some patients with tracheostomies, particularly in the immediate post op period, require humidity (RCH, n.d.). Humidification may also help to prevent ulceration of the tracheal mucosa, sputum retention, atelectasis, impaired gas exchange, and secondary infection (BTS, 2014).
- To optimize respiratory function and oxygenation, care should include physio, mobilization, hydration, suction, and medications as appropriate (BTS, 2014).
- New tracheostomies require attention to principles of asepsis for stoma (wound) care. Tracheostomies that are well established require clean technique for stoma care.
Potential Complications Associated with Tracheostomies
Early potential complications post tracheotomy may include hemorrhage, pneumothorax, subcutaneous emphysema, cuff leak, tube dislodgement, and respiratory/cardiovascular arrest. Complications occurring later, after the tracheostomy is established, may include airway obstruction, fistulae, infection, aspiration, and tracheal damage/erosion. Table 10.3 outlines potential complications, prevention strategies and interventions if the complication does occur.
Table 10.3 Potential Complications Associated with Tracheostomies, Prevention and Interventions |
||
Complication |
Prevention |
Interventions |
| Hemorrhage |
|
|
| Stomal / pulmonary infection |
|
Wounds are often kept moist by secretions and/or humidity. Moisture impairs healing.
Closed (in line) suction technique does not require sterile gloves. Humidity and hydration help to liquefy secretions for easier expectoration. Report potential signs of infection:
Routine instillation of NS to promote expectoration is not considered best practice. |
| Tube occlusion |
|
The inner cannula is a safety feature, and can be removed if occlusion occurs. Whenever possible use double lumen tubes for this reason.
If tube occludes:
|
| Aspiration |
|
High Fowler’s positioning promotes lung expansion. During swallow assessment, helps to reduce risk of aspiration if the patient begins to choke.
Report any signs of aspiration:
If patient vomits:
|
| Accidental decannulation |
|
If partial decannulation occurs (air movement is felt from tube):
If complete decanulation occurs, call for trained health care professional to reinsert tracheostomy tube. In the meantime:
|
| Note: Do not hyper-extend neck if patient has a known or suspected neck injury. | ||
| Data sources: BCIT, 2015b; BTS 2014; Vancouver Coastal Health, 2012a | ||
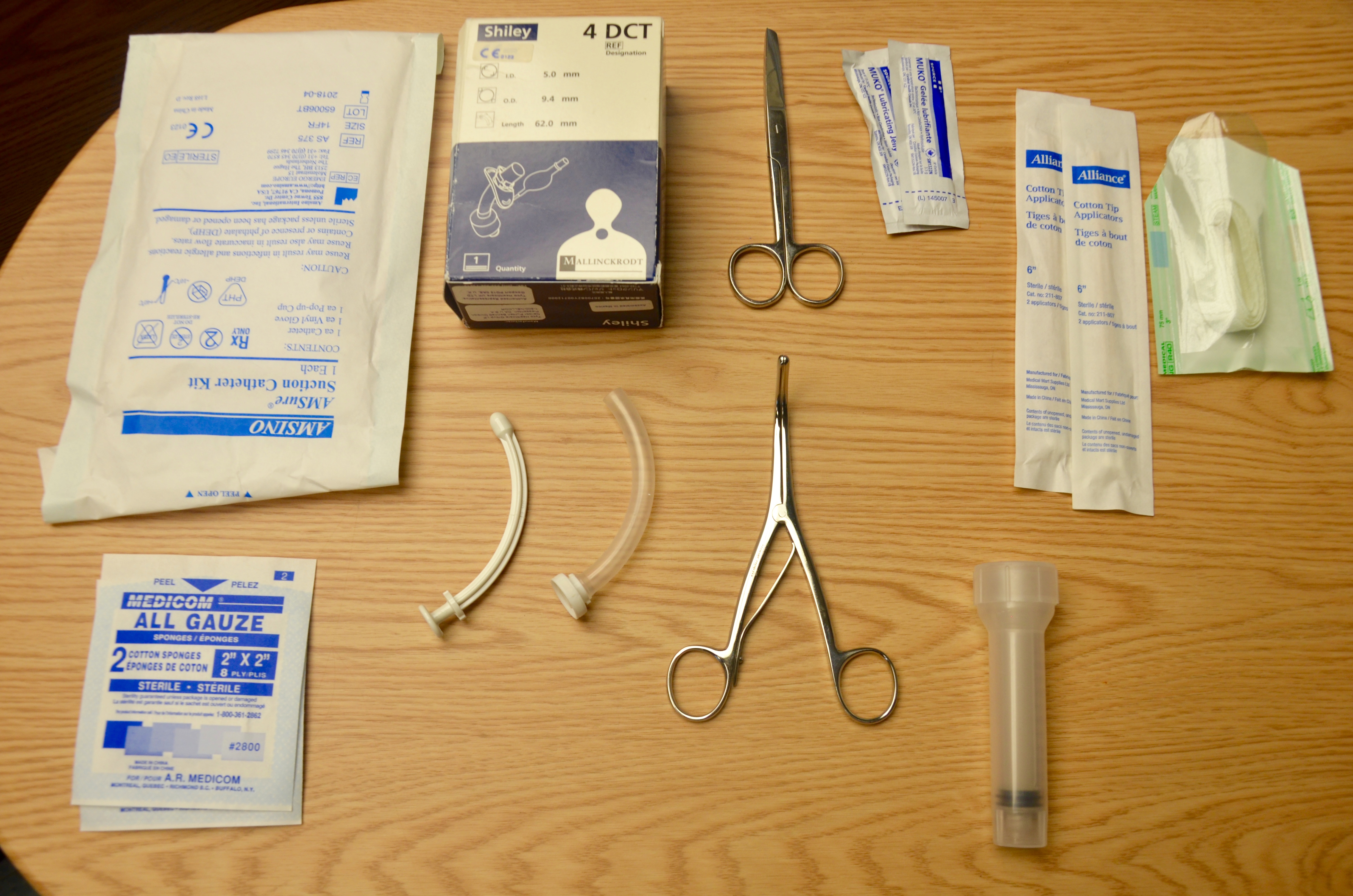
Emergency equipment should be available at the bedside and should accompany the patient off the unit. Check the agency policy to confirm contents. A basic kit should include:
- Suction equipment (portable unit if necessary).
- Oxygen equipment with humidification.
- An emergency bag containing (see Figure 10.6):
- Two replacement tracheostomy tubes (one of the same size, and one a smaller size than the current tube)
- Obturator and spare inner cannula
- 10 ml syringe
- Tracheal dilators
- Sterile gloves
- Water-soluble lubricant
- Scissors
- Cotton tip applicators
- Trach ties
- Sterile gauze
- Resuscitation bag and mask (appropriate size for patient)
Tracheostomy Care
Tracheostomy care is performed routinely and as required. Tracheostomy care is essential to avoid potential complications such as obstruction and infection. In addition to suctioning, tracheostomy care includes: changing, cleaning and replacing the inner cannula; changing the site dressing; and replacing the tracheostomy ties.
If possible, these three tasks of tracheostomy care should be performed at the same time to minimize handling of the tracheal device. Collect all supplies at once and complete the procedure in the order listed above. However, there may be times when each task may be performed separately. Ongoing assessment is essential when caring for a patient with a tracheostomy. Checklists 84-87 provide guidelines to do these things.
Additional care includes performing more frequent respiratory assessments and checking patency of tracheostomy tube to assess if suction is required (every two hours, and as needed) according to agency policy; keeping patient well hydrated (helps keep secretions thin); encouraging deep breathing and coughing (as required); reporting potential problems such as swelling, elevated temperature, change in sputum production, and decreasing or increasing O2 requirements.
Tracheal Suctioning
The purpose of suctioning is to maintain a patent airway, to remove secretions from the trachea and bronchi, and to stimulate the cough reflex (Vancouver Coastal Health, 2006). Patients with tracheostomies often have more secretions than normal and will require suctioning to remove secretions from the airway to prevent airway obstruction. People with a tracheostomy should be assessed frequently to determine if suctioning is required. In hospital, sterile suction equipment is used each time tracheal suctioning is performed unless you are using an in line suction catheter which can be used for several suction procedures (Perry et al., 2018). In the home environment, it is common and accepted practice to use “clean” rather than sterile technique during suctioning. The basis of this being that home microorganisms are a part of the person’s normal flora and less likely to make them sick (Lewarski, 2005).
Tracheal suctioning is indicated with noisy (moist) respirations, decreased O2 sats, anxiousness, restlessness, increased respirations or work of breathing, change in skin colour, or wheezing or gurgling sounds. These are signs and symptoms of respiratory distress, and the patient should be suctioned immediately. Checklist 84 outlines the steps for tracheal suctioning.
Checklist 84: Tracheal Suctioning—Open MethodDisclaimer: Always review and follow your agency policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Assess need for suctioning including respiratory assessment, signs of hypoxia, excess secretions, or alterations in oxygen levels. | Perform baseline respiratory assessment including SpO2.
Determine if the patient is on any medications that increase risk of bleeding. |
||
| 2. Explain the procedure in a calm, reassuring manner explaining the benefits are to remove secretions and to make breathing easier.
Position the patient in semi to high Fowler’s unless contraindicated. Drape chest with towel or disposable pad. |
Procedure can cause patient anxiety. This is part of the consent procedure.
Positioning promotes lung expansion and promotes secretion clearance. |
||
| 3. Perform hand hygiene. Gather equipment.
|
Equipment should include suction canister, regulator, suction tubing, sterile suction catheter, water soluble lubricant, PPE (face shield, sterile gloves, gown), sterile saline or water, and pulse oximeter.
Preparing equipment ahead of time promotes safety, organization, and timeliness. |
||
| 4. Administer oxygen if needed. This includes hyper-oxygenating if necessary. | Hyper-oxygenating might be necessary if the patient is hypoxic or at risk of hypoxia during procedure. | ||
| 5. Turn the suction device on, and set the vacuum regulator to the appropriate negative pressure. Set suction levels to medium / moderate.
Attach the suction catheter to the tubing whilst remaining in the sterile package. Open the sterile water / saline.
|
  Suction setting:
Excessive negative pressure damages mucosa and induces greater possibility for hypoxia. |
||
| 6. Perform hand hygiene and perform point of care risk assessment. Donne PPE.
|
At minimum, PPE should include face shield and gloves (gown is highly recommended). This prevents transmission of microorganisms to healthcare provider.
Sterile gloves in acute care environments. Clean gloves in home environments. |
||
| 7. Sterile procedure: Apply sterile gloves
With the non-dominant hand, pick up the packaged connecting tubing. That hand is now contaminated. Expose the suction catheter enough to allow the dominant hand (sterile) to grab the sterile catheter. Wrap the sterile catheter around the dominant hand. Suction a small amount of sterile NS / water. |
 You can also apply a non-sterile glove to the non-dominant hand and a sterile glove to the dominant hand. There is more than one way to remove the catheter from the packaging. The principle of sterile to sterile must apply to the tip of the suction catheter.  Suctioning sterile NS / water ensures properly functioning equipment. |
||
| 8. Insert suction catheter into tracheostomy until resistance is felt, then pull back about 1 cm. Do not apply suction when inserting suction catheter. |
 Resistance is felt at the level of the patient’s carina. |
||
| 9. Apply intermittent suction as the catheter is withdrawn. This means occluding and releasing the catheter vent with the non-dominant thumb. Some sources suggest twist the catheter back and forth as the catheter is withdrawn. Always encourage the patient to cough. | Do not apply suction for longer than 15 seconds. Suction removes oxygen and increases the risk of hypoxia as oxygen is sucked out.
The need to rotate the catheter is questioned in the literature because present day suction catheters have multiple eyes / holes. Encourage coughing to promote secretion clearance. Routine installation of normal saline into the trachea to loosen and mobilize secretions is not best practice. If a sterile sputum sample is required, follow agency policy for specific directions related to type of equipment in the agency. |
||
| 10. Replace oxygen delivery device and encourage deep breaths. | Promotes oxygenation. | ||
| 11. Clear secretions from suction catheter by suctioning sterile normal saline or water from sterile container. |
 Clears tubing of secretions to maintain patency. |
||
| 12. Assess need to repeat the procedure. Reassess respiratory status and O2 saturation for improvements. | Allow periods of rest between suction. The length of time between suctioning depends on patient tolerance. Patient may be suctioned up to three times with the same suction catheter. Do not pass (insert) suction catheter more than three times.
Declining SpO2 suggests the patient is not tolerating the procedure. Consult the prescriber and/or respiratory therapist. Call for help if any abnormal signs and symptoms appear, or if respiratory status does not improve. |
||
| 13. Discard suction catheter, sterile saline / water, and sterile gloves. Turn off suction. Remove gloves. Perform hand hygiene.
Ensure supplies are readily available at the bedside for next suction procedure. |
Open suctioning method requires new suction catheter after each round of suctioning. Reuse may introduce microorganisms into the patient’s respiratory tract increasing risk of infection.
 Additional suction supplies are essential in case of an emergency or respiratory distress. |
||
| 14. Return patient to a safe and comfortable position and ensure that call bell is within patient’s reach. | This promotes patient safety. | ||
| 15. Document procedure according to agency policy. | Documentation may include the suction procedure; patient reaction; amount, thickness, and color of secretions; if normal saline was instilled; and if sputum samples were sent to the lab. Documentation provides accurate details of response to suctioning and clear communication among the health care team.
Sample narrative documentation: date / time: Audibly moist respirations. Thick yellow tinged secretions observed at trach site. T 37.5 HR 98 RR 24 BP 146/79. SpO2 90% on 40% humidified oxygen @ 10L/ min. Trach suctioned with #14 suction catheter for moderate think yellow secrrtions. Cough reflex apparent. Following procedure RR 20/min. SpO2 98%. O2 reestablished as noted above. —— L,Owox RN |
||
| Data sources: BCIT, 2015c; Halm & Krisko-Hagel, 2008; Perry et al., 2018; Vancouver Coastal Health, 2006 | |||
A closed method of tracheal suctioning involves a multi-use suction catheter enclosed in a plastic sleeve and attached to the patient’s airway (tracheal tube). In comparison to the open suction method, the closed method presents less risk of hypoxia and cardiovascular complications. To initiate closed suctioning, consult a respiratory therapist.
Replacing and Cleaning an Inner Tracheal Cannula
The primary purpose of the inner cannula is to prevent tracheostomy tube obstruction. Many sources of obstruction can be prevented if the inner cannula is regularly cleaned and replaced. The inner cannula can be cleansed with half-strength hydrogen peroxide or sterile normal saline. Always check the manufacturer’s recommendations for tube cleaning. Some inner cannulas are designed to be disposable, while others are reusable for a number of days. Inner tube cleaning should be done as often as two or three times per day, depending on the type of equipment, the amount and thickness of secretions, and the patient’s ability to cough up the secretions.
Changing the inner cannula may encourage the patient to cough, bringing mucous out of the tracheostomy. For this reason, the inner cannula should be replaced prior to changing the tracheostomy dressing to prevent secretions from soiling the new dressing. If the inner cannula is disposable, no cleaning is required. Checklist 85 describes how to clean and replace an inner tracheal cannula.
Checklist 85: Replacing and Cleaning an Inner Tracheal CannulaDisclaimer: Always review and follow your agency policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Perform hand hygiene, collect supplies, and verify whether inner cannula needs to be cleaned as per policy. | Supplies include cotton-tip applicator, sterile pipe cleaner, sterile dressing tray, NS, non-sterile gloves, waterproof pad, and PPE. | ||
| 2. Perform hand hygiene, ID patient using two identifiers, explain procedure to patient, and create privacy if required.
Ensure patient has a method to communicate with you during the procedure. |
Hand hygiene reduces the transmission of microorganisms.
People with tracheostomies require a method to communicate with the healthcare provider. |
||
| 3. Apply gloves and PPE , and cover chest with waterproof pad. | This prevents contact with secretions and prevents gown from becoming soiled.
Use sterile technique in acute care, clean technique in home environments. |
||
| 4. Set up sterile tray field; add cleaning solution and supplies. | Organization ensures the process is efficient and fast for the patient.
 |
||
| 5. Remove oxygen mask to clean dressing, but replace frequently as required by patient. |
 Replace the tracheal oxygen mask frequently to prevent hypoxia. |
||
| 6. Remove inner cannula by stabilizing neck plate / flange and gently grasping the outer white area. Rotate inner cannula counter-clockwise to unlock it. Pull cannula out in a downward motion. Some inner cannulae will “click” on, some twist on/off. Do not touch the inner cannula; only handle the white outer area unless you are wearing sterile gloves.
Replace the client’s oxygen while cleaning the inner cannula to prevent the client from desaturating or drying out secretions |
Review policy for cleaning frequency and cleaning solution.
 |
||
| 7. Soak inner cannula in saline, if necessary, use a sterile pipe cleaner or cotton tipped applicators with gauze to remove exudate from the inner lumen. Rinse well. | Soaking the cannula helps loosen the secretions.
 |
||
| 8. Reinsert inner cannula by stabilizing neck plate, holding the white part with the end upright, and twisting into the shape of the tracheostomy. | This prevents trauma to the tracheal stoma. | ||
| 9. Ensure the inner cannula has “clicked” into place. Use sterile gauze to clean the outer cannula surfaces |
 |
||
| 10. Discard used equipment. Remove gloves. Perform hand hygiene.
Ensure the patient is in a safe and comfortable position. |
Hand hygiene reduces the transmission of microorganisms. | ||
| Data sources: BCIT, 2015c; Morris, Whitmer, & McIntosh, 2013; Perry et al., 2018; Vancouver Coastal Health, 2012b | |||
Cleaning Stoma and Changing the Tracheosotomy Site Dressing
The stoma should be cleaned and the dressing changed every 6 to 12 hours or as needed, and the peristomal skin should be inspected for skin breakdown, redness, irritation, ulceration, pain, infection, or dried secretions. Patients with copious amounts of secretions often require frequent dressing changes to prevent maceration of the tissue and skin breakdown. Cotton-tip applicators can be used to get under the tracheostomy device, where cleaning can be done using a semi-circular motion, inward to outward. Always use aseptic technique. Checklist 86 provides a safe method to clean the tracheal stoma and replace the sterile dressing.
Tracheal ties will become dirty and require replacing. Ties should be replaced as required, according to agency policy. Ideally, one person should hold the tracheostomy tube in place while the tracheostomy ties are replaced by another person. Alternatively, secure the new tracheostomy ties prior to removing the old tracheostomy ties to avoid accidental dislodgement of the tracheostomy tube if the patient coughs or the tracheostomy is accidentally bumped out. Once the new tracheostomy ties are on, only one finger should fit between the tracheostomy ties and the neck.
Replacing Tracheostomy Ties (Velcro)
Checklist 87 lists the steps for replacing tracheostomy ties.
Checklist 87: Replacing Tracheostomy Ties (Velcro)Disclaimer: Always review and follow your agency policy regarding this specific skill. |
|||
Safety considerations:
|
|||
Steps |
Additional Information |
||
| 1. Perform hand hygiene, collect supplies. Assess need for PPE | Hand hygiene reduces the transmission of microorganisms.
Supplies include twill or Velcro ties, a second person to secure the tracheostomy when old ties are removed, scissors if using twill tape ties. |
||
| 2. Have an additional health care provider assist with the tracheal tie change as required. | An additional helper is there to secure the trachestomy tube and prevent accidental dislodgement. | ||
| 3. ID patient using two identifiers, explain procedure to patient, and create privacy if required. Ensure patient has a method to communicate with you during the procedure. | Persons with a tracheostomy require a method to communicate with the health care provider. | ||
| 4. Apply non-sterile gloves. | This reduces the transmission of microorganisms. | ||
5. To secure the tracheostomy tube with velcro ties:
|
Tracheostomy ties are used to promote patient comfort and keep the tracheostomy secured and in situ.
An assistant can hold the trach tube in place to reduce risk of potential dislodgement of the tube if the patient coughs.  The tape should be tight enough to keep the tracheostomy tube securely in place but loose enough to allow the little finger to fit between the tapes and the neck. |
||
| 6. Clean the work area. Discard garbage appropriately. Perform hand hygiene. Leave the patient in a comfortable position. | Hand hygiene reduces the transmission of microorganisms. | ||
| Data sources: BCIT, 2015c; Morris et al., 2013; Perry et al., 2018 | |||
Critical Thinking Exercises
- When suctioning your patient who has a tracheostomy, you notice thick, tenacious secretions. What interventions should be implemented?
- What methods of communication can you use for your patient with a tracheostomy tube who is unable to speak?
- Answer yes or no in relation to whether or not each of the following situations presents a concern:
a) If a person has a cuffed tracheostomy in place requires manual ventilation, such as with a bag and mask via the nose, will this deliver oxygen to the patient?
b) A suction catheter cannot pass through a tracheostomy.
c) A patient with an tracheostomy tube that has an inflated cuff is able to talk.
d) Decannulation occurred 4 days ago. The occlusive dressing has fallen off. The wound is now closed.
Attributions
Figure 10.1. Untitled by pixabay.com is used under an open Pexels license.
Figure 10.2. Tracheostomy Tube by Klaus D. Peter is used under a CC BY 2.0 DE license.
Figure 10.3 & 10.4. These are modified reproductions of “Diagram of an inserted endotracheal tube” by PhilippN in the Public Domain / A derivative from the original work.
Figure 10.5. Diagram Showing a Fenestrated and a Non Fenestrated Tracheostomy Tube by Cancer Research UK is used under a CC BY-SA 4.0 international license.
Figure 10.6 Emergency equipment is from BCIT
Figure 10.7 WAll suction unit by author is





